Many men with prostate cancer didn’t need treatment, yet most still had surgery or radiation, hindering widespread screening adoption.
A study published in JAMA Oncology revealed that between 2010 and 2024, the number of patients with the lowest-risk prostate cancer undergoing prostatectomy declined more than fivefold. ()
What is Prostatectomy?
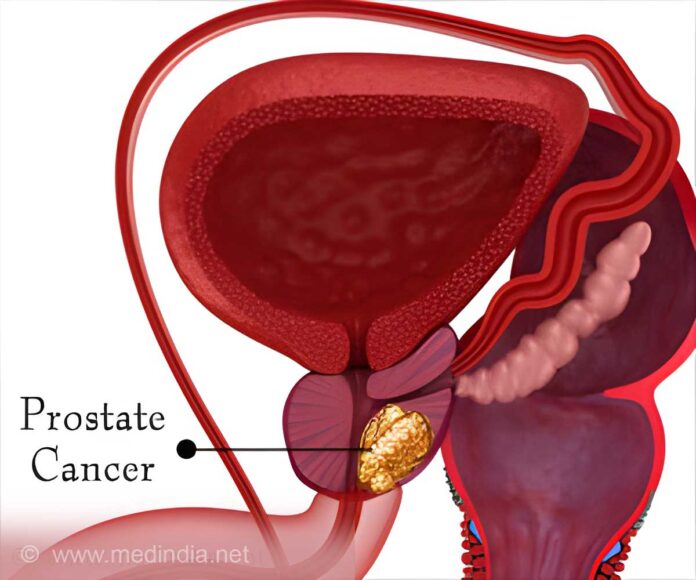
A prostatectomy is a surgical procedure used to remove all or part of the prostate gland, most often to treat prostate cancer or, in some cases, an enlarged prostate. There are several types of prostatectomy, including radical, simple, open, and robotic-assisted, depending on the condition being treated and the surgical approach.
The primary goal is to eliminate cancer while preserving urinary and sexual function as much as possible. Recovery time varies by procedure and individual, and some patients may experience side effects such as incontinence or erectile dysfunction.
Prostate cancer remains one of the top causes of cancer-related deaths among men in the U.S. However, routine screening for the disease has sparked debate. Many primary care physicians are concerned it may result in unnecessary surgeries for men with low-risk cases, prompting current guidelines to recommend screening only after patients are informed about the potential risks of overtreatment.
However, not all prostate cancers are the same. Some grow so slowly that they’re unlikely to ever cause problems, especially in older men. “The discrepancy between how common prostate cancer is and the hesitance in adopting screening exists because, historically, prostate cancer has been considered overtreated,” said Steven Monda, M.D., urologic oncology researcher and first author of the study.
In 2012, the U.S. Preventative Task Force recommended against routine screening of prostate-specific antigen, or PSA, levels due to concerns about overtreatment. Prostate cancer in many men does not require treatment. However, in the past, most of these men still underwent surgery or radiation after their diagnosis, which led to hesitance in the widespread adoption of screening.”
This stance was softened in 2018 to allow PSA screening only after patients discussed the risks and benefits with their doctor. “Even though the 2012 USPTF guidelines were revised, many primary care doctors never went back to screening,” said Tudor Borza, assistant professor of urology and senior author on the study.
“As a result, even people at a higher risk, such as African American men or those with a family history of prostate cancer, aren’t being offered screening.” In the current study, the group analyzed data from over 180,000 men who had prostate cancer surgery between 2010 and 2024.
They focused on patients with Grade Group 1 prostate cancer, which is the lowest-risk category. These are the men most likely to be good candidates for active surveillance, an approach in which doctors monitor the cancer with regular tests and intervene only if it worsens.
Using two prostate cancer registries—one national and one based in Michigan—the researchers showed that the proportion of patients undergoing prostatectomy for the lowest risk type of cancer dropped over fivefold from 2010 to 2024. In 2010, one in three men who had prostate cancer surgery nationally had the low risk type. By 2020, that number dropped to less than one in 10.
In Michigan, where urologists have been working for years on quality improvement through a program called MUSIC, the proportion dropped from about one in five in 2012 to less than one in 35 in 2024. The study also found that, across different surgical practices throughout the state, rates of unnecessary surgery declined consistently.
“The results who that this is a system-wide improvement,” Monda said. “We’re seeing progress at the local practice, statewide and national levels.” These results align with other studies that showed increased use of active surveillance for low risk prostate cancer since 2010.
“The decrease in the number of surgeries for low-grade prostate cancer shows that active surveillance helps,” Monda said. “Routine PSA checks, MRIs and biopsies can ensure that prostate cancer doesn’t progress to a condition that requires treatment.”
Reference:
- Trends in Surgical Overtreatment of Prostate Cancer – (https://jamanetwork.com/journals/jamaoncology/fullarticle/2833303?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamaoncol.2025.0963)
Source-Newswise